Perth's Leading Specialist in the Treatment of Varicose Veins
Dr Luke Matar | MBBS, FRANZCR, FACP
What is Glue Treatment For Veins?
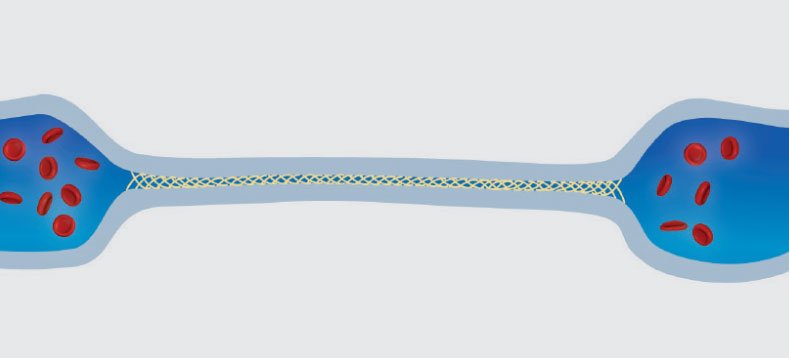
The most well known and used glue treatment for veins in Australia is the VenaSeal™ closure system. It was developed to improve the patient experience in the treatment of varicose veins and aims to replace the need for surgery, Endovenous Laser Ablation or Radiofrequency Ablation in many cases of saphenous insufficiency, by using a cyanoacrylate adhesive or “medical superglue” to seal the abnormal vein.
How Does Glue Treatment Work?
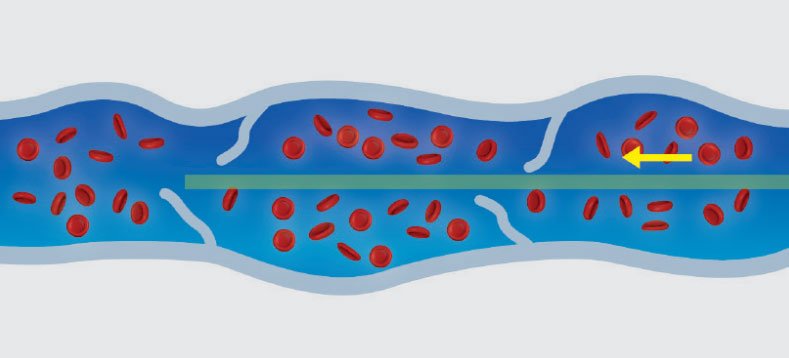
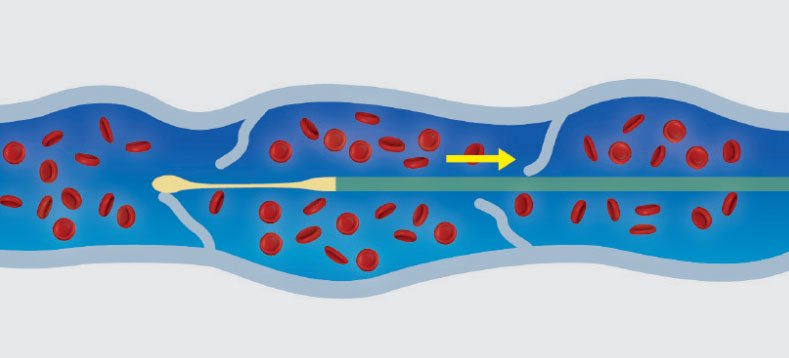
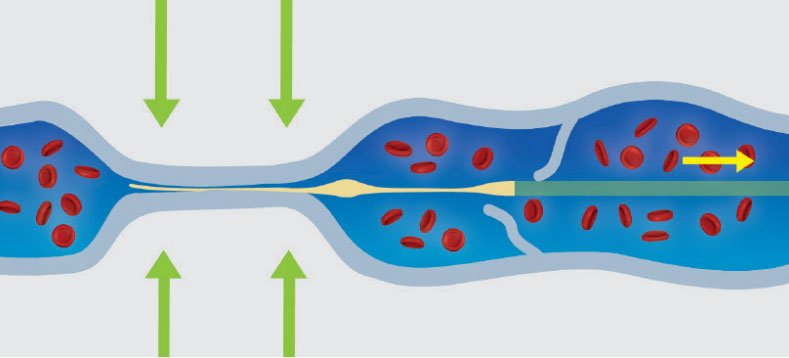
The VenaSeal™ procedure involves the placement of a very small amount of cyanoacrylate adhesive (medical superglue) into the abnormal vein through a catheter delivery system.
Whilst the initial studies suggested this to be equally affective as laser and a be a “painless procedure” without the need for the wearing stockings, this has not always been our experience.
How Long Has Glue Treatment Been Around For?
CE mark approval (Europe) occurred in September 2011, Australian TGA approval in January 2012 and US Food and Drug Administration (FDA) approval in February 2015. MBS (Medicare) funding for this procedure was introduced in May 2018.
Glue Treatment
Before & Afters
Treatment Method
These before/after images demonstrate a case study of glue treatment for veins. A 59-year-old patient presented with large varicose veins after 20 years of discomfort and heavy legs toward the end of the day, as well as symptoms of itchy legs. As a cabinet maker, he wanted a tailored “walk-in walk-out” treatment approach that would allow him to go back to work ASAP with minimal downtime.
The first stage of treatment involved VenaSeal glue treatment to the malfunctioning saphenous veins. The second stage included sclerotherapy and ultrasound-guided phlebectomy removal of branch vessels.
The Procedure
How Safe is Glue Treatment?
Cyanoacrylate-based medical glue, a time-tested adhesive employed in medical practices such as brain surgery and wound closure for over 50 years, boasts an impressive safety record. Initial studies involving cyanoacrylate for vein treatment suggested that severe adverse events were comparatively rare.
However, new perspectives have been brought to light by a pivotal presentation by Professor Parsi, Head of UIP, at the 2023 Adelaide ACP (Australiasian College of Phlebology) conference. His research highlights potential complications linked with glue treatment for veins, pinpointing risks tied to potential allergies to the glue’s components and subsequent foreign body reactions. This revelation underscores the significance of ongoing research and a comprehensive understanding of vein treatment options.
As a result of this recent evidence, alongside emerging literature and reports of adverse events listed on the FDA website, Dr. Matar has reevaluated the risk-benefit balance of glue treatment for saphenous veins. Given the outstanding efficacy of laser treatment, which avoids the unique risks associated with glue, Dr. Matar now predominantly favours laser as the primary method for treating saphenous veins.
Is Glue Treatment The Right Option For You?
Should you be considering glue treatment for varicose veins, it’s crucial to familiarise yourself with the recognised risks and benefits of this procedure. As this method is relatively recent, our understanding continues to evolve. Certain risks we are aware of today were not known when cyanoacrylate glue was initially licensed for use both in Australia and internationally.
Reflecting on the perspectives of phlebology professionals, a significant shift is apparent. Most phlebologists in Australia and New Zealand no longer employ glue for saphenous vein closures, a marked contrast from the scenario five years ago when the majority advocated its use.
Read MoreWhy Choose The Vein Clinic Perth?
Dr Luke Matar’s journey in the specialised field of phlebology began in 2011 with UK-based EVLA expert Professor Mark Whiteley, renowned as the inventor of laser perforator vein ablation. Following this, Dr Matar honed his expertise under the guidance of several international vein specialists, including Professor Kurosh Parsi, Professor Ken Myers, Dr Mark Malouf, Dr Andrew Stirling, Dr Loius Loizou, Dr Chris Lekich, Dr Chris Ragg (Berlin) Dr David West (UK) and Dr Ron Bush (USA).
Dr Matar established the Vein Clinic in 2014, driven by the desire to offer world class vein treatments to his patients. His practice philosophy is deeply personal: providing the kind of treatment he would wish for himself or a family member. This means recommending what is genuinely best for the patient, even if it requires referring them elsewhere for particular vein issues.
Having personally undergone three laser treatments, multiple phlebectomies and foam sclerotherapy sessions, Dr Matar empathises deeply with his patients’ experiences. His passion and commitment lie in offering individualised treatment plans, uniquely customised to address each patient’s specific vein issues and personal preferences. The unique insight gained from the other side of the treatment table also led him to refine and pioneer a number of advanced treatments including UGFP (Ultrasound-Guided Foam Phlebectomy) and extended endovenous laser ablation pushing the boundaries of what can be achieved with laser treatment alone.
Do I Need Treatment for Varicose Veins?
You could benefit from treatment for varicose veins if you experience any of the following vein problems.
Other Minimally Invasive
Varicose Veins Treatments
Frequently Asked Questions
Why do I have varicose veins?
Most varicose vein issues are hereditary. If you have one parent with varicose veins your risk of having them is around 65%. If both parents are affected the risk rises to approximately 90%. Another main risk factor for women is pregnancy, with the risk increasing with each additional pregnancy. Standing occupations such as hairdressers, nurses, and chefs also have a high risk of varicose veins as gravity puts pressure on the veins and weakens them.
How do I prevent varicose veins?
Once varicose veins are present, they will not resolve of their own accord. Measures to reduce the rate of progression include maintaining a normal healthy weight and going for regular walks of 20-30 minutes per day. Reducing the length of time spent on the feet in a stationary position may help and alternating between standing and sitting positions during the day will also reduce the pressure on the veins.
What will happen if I don’t treat these veins?
Generally, without treatment, varicose veins will get progressively worse over time. Symptoms may occur such as heaviness, ache, pain, and tiredness in the legs towards the end of the day. Further progression may result in leg swelling, itch, skin discolouration, and eventual skin ulceration. Blood clots related to superficial venous thrombosis may also occur in severe cases and can lead to the more serious condition of Deep Vein Thrombosis.
What treatment options exist?
Outdated, old-fashioned options such as surgical stripping are rapidly becoming obsolete due to poor long-term success, with recurrence rates of up to 50%. Modern treatment options include endovenous laser ablation, sclerotherapy injections, and ultrasound-guided ambulatory phlebectomy. In many cases a combination of different treatments will give the best long-term results.
Will the veins come back after treatment?
Many people are concerned that the treatment will be of limited value because the veins will just come back. This was certainly the case in the days of surgical stripping with a 50% recurrence rate at 5 years; however, using the latest minimally invasive techniques, we can reduce the risk of recurrent varicose veins to the baseline risk of approximately 3% per year.
What is the downtime following treatment?
This depends on the type of procedure performed and the severity of the veins being treated. Modern treatment with laser can involve no time off work and approximately two weeks off heavy gym work and four weeks off international travel.
Get In Touch
Please send us an email and we’ll be in contact very soon or alternatively, call us on (08) 9200 3450.
If you are unsure of what vein condition you may have, assess your legs with our online tool.
If you are looking for cosmetic spider vein treatment only, please click here.